- Introduction
- Purpose of the Foundation Programme
- Progression through Foundation Training
- How to use the Curriculum in the Workplace
- Resources: foundation doctors
- Resources: trainers, supervisors and placement supervision group
- The educational framework and recognising learning styles
- Educational framework
- Educational culture and practice
- How to use the Syllabus
- Learning and teaching
- Supervised learning events (SLEs)
- Assessment
- Syllabus
- Bibliography
- Appendices
- Download
Appendicies
Appendix A
Changes since 2012 (including minor curricular changes for 2014 and 2015) and future development
This planned revision of the foundation programme curriculum has been undertaken as an evolutionary process and has been performed with input and feedback from many stakeholders. During the revision, there has been dialogue between representatives from the Academy of Medical Royal Colleges (AoMRC) Foundation Programme Committee, UK Foundation Programme Office (UKFPO) and General Medical Council (GMC) to ensure that changes are deliverable and that the regulator is aware of the nature of the revisions to ensure that they are in keeping with regulatory requirements.
This revision continues to reflect suggestions made in Foundation for Excellence: An Evaluation of the Foundation Programme report (2010) in particular in relation to refinement of the assessment process.
As a prelude to the revision process, feedback on the foundation programme curriculum was sought from a wide range of stakeholders (Appendix D) both by direct invitation (key stakeholders and organisations/ individuals who had previously expressed interest in the foundation programme curriculum) and by general invitation through the Academy of Medical Royal Colleges website. Extensive feedback was received, this was collated and emerging themes were identified. The curriculum working group reviewed the collated evidence and made revisions to the curriculum accordingly. There was a clear message of support for the changes made in 2012 and a request that changes introduced for 2016 should be evolutionary.
Impact of these changes to the curriculum
Although the 2016 curriculum will be a web-based document, the overall layout of the new curriculum will be instantly recognisable to those familiar with the 2012 curriculum. Existing users should be able to make a straightforward transition to use the 2016 curriculum.
Structural changes in the curriculum
The following noteworthy structural changes have been made:
Reorganisation of the syllabic component to reflect better the ethos of Good Medical Practice 2013 and Promoting Excellence: Standards for medical education and training 15 July 2015.
The 2016 syllabus comprises four sections compared to two sections in 2012.
Section 1: Professional behaviour and trust
Section 2: Communication, team working and leadership
Section 3: Clinical care
Section 4: Safety and qualityCurriculum outcomes have been reduced to 20, these are termed foundation professional capabilities. New high-level terms have been introduced to indicate the minimum level of performance expected from doctors in F1 and F2. Progression to the next stage of training at the end of F1 and F2 is dependent on the foundation doctor demonstrating that they have met or exceeded the minimum levels of performance required for sign off for each of the 20 foundation professional capabilities (foundation programme training outcomes). This continues the evolution to reduce the burden of assessment and to make the assessment process more meaningful which began in 2012.
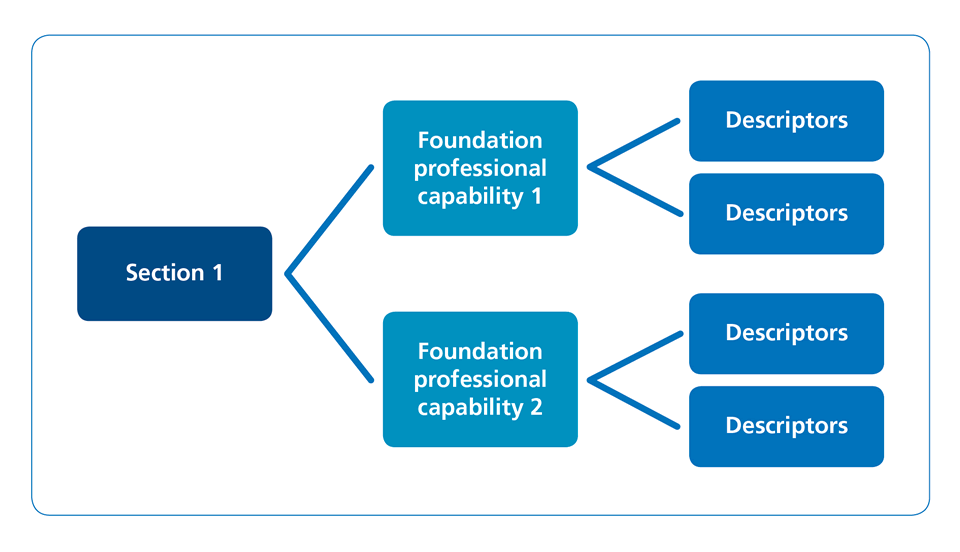
'Descriptors' are provided these are general expectations and indicative examples of clinical and professional accomplishments related to the associated 'foundation professional capability'. Many of these 'descriptors' will be familiar having been derived from the outcomes used in the 2012 curriculum. The vast majority of outcomes have been retained but all have been reviewed to reflect feedback, ensure that they are contemporary and to reduce duplication.
Competences have been removed from the curriculum.
The syllabus hierarchy can be understood from the following schematic:
Reorganisation and revision of the introductory sections and appendices. These have been reordered to improve accessibility at the suggestion of the foundation school directors. The explanatory sections relating to how to use the curriculum are clearer and reflect the changes introduced for 2016. All changes to the curriculum are explained in the introductory section and appendices.
Assessment
The processes and timings assessment within the foundation programme have not changed and remain:
- The clinical supervisor's end of placement report
- The educational supervisor's end of placement report
- Team assessment of behaviour
- Evidence of proficiency in the GMC mandated procedures (F1 only)
- The educational supervisor's annual report
- The annual review of competence progression.
The minimum level of performance expected from a trainee at the end of each year of training is clearly. The end of placement reports will indicate whether the foundation doctor's performance is on course to meet or exceeded the minimum levels of performance required for sign off for each of the 20 foundation professional capabilities (foundation programme training outcomes) by the ARCP process at the end of the year of training.
The educational and clinical supervisor's reports will now comment on performance at section level based on evidence of achievement for each of the 20 professional capabilities (foundation programme training outcomes). The report will indicate whether performance is on course to meet or exceeded the minimum levels of performance required for sign off for each of the 20 foundation professional capabilities The clinical supervisor's judgment will continue to be informed by direct observation of the foundation doctor in the workplace, feedback from the placement supervision group, evidence of engagement with the learning processes defined in the curriculum and evidence of achievement of curriculum outcomes from the e-portfolio.
Foundation doctors will continue to demonstrate their achievements using a range of evidence including: reflection on clinical or professional experiences, evidence of formal training (certificates), participation in evidence based medicine (guidelines, posters, presentations) or quality improvement work.
The totality of engagement in populating the various domains in the e-portfolio will continue to be used as a method of assessment of the doctor's success in achieving the outcomes described in the curriculum.
The ratings used in the clinical and educational supervisor's reports have been revised and will be: no concern, minor concern, major concern. Comments in support of the judgement are mandatory. Whenever there is concern, specific comments must be made regarding any of professional capabilities (foundation programme training outcomes) where there are performance issues. Further detail based on the 'descriptors may also be referenced.
The educational and clinical supervisor report forms have been streamlined and the associated guidance documentation has been revised to reflect these changes.
Syllabus
There has been comprehensive review of the syllabus, which has been reorganised as described above.
Five important themes emerged from the stakeholder feedback: mental health, frailty, protection of vulnerable groups, mental capacity act, end of life care. Each of these areas of the syllabus has been comprehensively revised and strengthened.
Curriculum outcomes now relate more closely to those in General Medical Practice (GMP) and Promoting Excellence: Standards for medical education and training.
The 'descriptors' relating to each of the professional capabilities are grouped under headings which reflect the feedback and are grouped more logically. Several new headings have been introduced relating to the key themes. Headings relating to specific syndromes have been removed from the syllabus. This is in keeping with the foundation programme's stated aims to provide generic training to provide safe and effective care for patients with acute and long-term conditions irrespective of the clinical context.
Although there are only 20 foundation professional capabilities (foundation programme training outcomes) to be evidenced in the 2016 curriculum the detail and granularity within the descriptors has been maintained. Thus it will be simpler for trainees to provide evidence of how their performance meets expectations for each of the 20 professional capabilities (foundation programme training outcomes) and simpler for supervisors to review achievement to judge performance. Conversely the retention of detail will ensure that it is possible to document issues in the case of a foundation doctor who is not making expected progress.
Additional comments from 2012
In 2012, the AoMRC undertook to assess the feasibility of including a patient feedback tool in 2016. A study was undertaken by the Picker Institute, which indicated that at present it was not feasible to collect meaningful patient feedback. In consequence, patient feedback is not incorporated in the 2016 curriculum.
The AoMRC has also assessed the impact of the introduction of supervised learning events. The results demonstrated that there was still incomplete understanding of the SLE tools but that where they were understood they were preferred to the workplace based assessments which they replaced. The extensive feedback received, indicated satisfaction with the assessment system.
Future development of the curriculum
There are no major structural changes planned. The curriculum will continue to evolve as a result of feedback. The move to a web based curriculum for 2016 will simplify the introduction of any minor changes required for patient safety purposes as this will not necessitate reprinting the curriculum.
Next scheduled full revision of the curriculum.
This is planned by 2021 at the latest but the 2016 curriculum will be reviewed and revised in line with General Medical Council regulatory requirements as necessary.
Appendix B
Ensuring quality in foundation programmes
The General Medical Council (GMC) is the competent authority in the United Kingdom with regard to European Union legislation for undergraduate and postgraduate medical education. Responsibility for the approval of the training provided in the foundation programme rests with the GMC as the regulator.
The foundation programme is regulated by the GMC, through its Postgraduate Board. The regulator has in place a robust quality assurance system, which is set out in the Quality Improvement Framework (QIF). Through the QIF, the GMC:
- Approves:
- Foundation schools/deaneries responsible for foundation training
- Local education providers delivering foundation training
- The foundation curriculum assessment system and foundation programme
- Maintains an evidence base of information from foundation schools/deaneries about foundation training, gathered through scheduled reports from foundation schools/deaneries every six months
- Carries out visits to quality assure foundation training as part of regional visits to foundation schools/deaneries
- Supports the development and improvement of local foundation programme education and training by ensuring that useful and innovative educational practices are shared (horizontal connections)
- Ensures that foundation training is aligned with undergraduate and postgraduate education (vertical connections).
i) Quality assurance - carried out by the regulatory authorities
Quality assurance encompasses all the policies, standards, systems and processes involved with ensuring maintenance and enhancement of the quality of postgraduate medical education in the UK. The regulator undertakes planned and systematic activities to provide public and patient confidence that postgraduate medical education satisfies given requirements for quality within the principles of good regulation.
ii) Quality management - carried out by the foundation school/postgraduate deanery
Quality management refers to the arrangements by which the foundation school/postgraduate deanery discharges its responsibility for the standards and quality of postgraduate medical education. The foundation schools/deanery must satisfy itself that local education and training providers are meeting the regulator's standards through robust reporting and monitoring mechanisms.
iii) Quality control - carried out at local education provider (LEP) level
Quality control relates to the arrangements (procedures and organisation) within local education providers (health boards, NHS trusts and independent sector organisations) that ensure postgraduate medical foundation doctors receive education and training that meet local, national and professional standards.
These processes are interdependent. The regulator's Quality Assurance is a systematic educational audit of the deanery quality management systems; the latter must include review of LEP quality control measures. The regulator has set national standards for the delivery and outcomes of the foundation programme and deaneries are required to demonstrate through reports and visits that the standards have been met.
There are nine domains of activity described:
- Patient safety
- Quality assurance, review and evaluation
- Equality, diversity and opportunity
- Recruitment, selection and appointment
- Delivery of the curriculum including assessment
- Support and development of foundation doctors, trainers and local faculty
- Management of education and training
- Educational resources and capacity
- Outcomes.
In each domain, the regulator has described who is responsible for its achievement, the standard(s) to be reached, and the criteria by which its achievement is judged. The standards set by the regulator are mandatory, but the processes by which deaneries quality manage, and LEP quality control, the programme provision are not specified.
Full information on the quality assurance of the foundation programme can be obtained from the GMC website.
Examples of 'good practice' in the implementation of the curriculum can be found on the UKFPO website.
Appendix C
Mapping the Foundation Programme Curriculum 2016 to GMC standards
The foundation programme curriculum has been mapped to the four domains of the Good Medical Practice, illustrating where the standards have been fulfilled in the curriculum syllabus.
Domain 1 - Knowledge, skills and performance
|
Attributes |
Generic standards |
FP Curriculum Syllabus Reference to Curriculum outcomes 1-20
|
|
Develop and maintain your professional performance |
|
4 |
|
4 |
|
|
4,5 |
|
|
4,5 |
|
|
|
|
1,2,3 |
|
|
|
3 |
|
|
|
4 |
|
Apply knowledge and experience to practice |
|
18 |
a) Adequately assess the patient’s conditions, taking account of their history (including the symptoms and psychological, spiritual, social and cultural factors), their views and values; where necessary, examine the patient. b) Promptly provide or arrange suitable advice, investigations or treatment where necessary. c) Refer a patient to another practitioner when this serves the patient’s needs. |
2,9, 10, 11, 12, 13, 14 and 15 |
|
a) Prescribe drugs or treatment, including repeat prescriptions, only when you have adequate knowledge of the patient’s health and are satisfied that the drugs or treatment serve the patient’s needs. b) Provide effective treatments based on the best available evidence. c) Take all possible steps to alleviate pain and distress whether or not a cure may be possible.. d) Consult colleagues where appropriate. e) Respect the patient’s right to seek a second opinion. f) Check that the care or treatment you provide for each patient is compatible with any other treatments the patient is receiving, including (where possible) self-prescribed over-the-counter medications. g) Wherever possible, avoid providing medical care to yourself or anyone with whom you have a close personal relationship. |
|
|
|
|
|
2 |
|
|
|
20 |
|
Record your work clearly, accurately and legibly |
|
6 |
|
2, 3 |
|
|
|
a) Relevant clinical findings. b) The decisions made and actions agreed, and who is making the decisions and agreeing the actions. c) The information given to patients. d) Any drugs prescribed or other investigation or treatment. e) Who is making the record and when. |
6 |
Domain 2 – Safety and quality
|
Attributes |
Generic standards |
FP Curriculum Syllabus Reference |
|
Contribute to and comply with systems to protect patients |
a) Taking part in regular reviews and audits of your work and that of your team, responding constructively to the outcomes, taking steps to address any problems and carrying out further training where necessary b) Regularly reflecting on your standards of practice and the care you provide c) Reviewing patient feedback where it is available. |
4, 18, 19 |
|
To help keep patients safe you must: a) Contribute to confidential inquiries. b) Contribute to adverse event recognition. c) Report adverse incidents involving medical devices that put or have the potential to put the safety of a patient, or another person, at risk. d) Report suspected adverse drug reactions. e) Respond to requests from organisations monitoring public health. When providing information for these purposes you should still respect patients’ confidentiality. |
3, 19 |
|
|
Respond to risks to safety |
|
6, 7, 9, 19 |
a) If a patient is not receiving basic care to meet their needs, you must immediately tell someone who is in a position to act straight away. b) If patients are at risk because of inadequate premises, equipment* or other resources, policies or systems, you should put the matter right if that is possible. You must raise your concern in line with our guidance and your workplace policy. You should also make a record of the steps you have taken. c) If you have concerns that a colleague may not be fit to practise and may be putting patients at risk, you must ask for advice from a colleague, your defence body or us. If you are still concerned you must report this, in line with our guidance and your workplace policy, and make a record of the steps you have taken. |
|
|
|
18 |
|
|
3,19 |
|
|
Protect patients and colleagues from any risk posed by your health |
|
1, 19 |
|
19 |
|
|
|
|
19
|
Domain 3 – Communication, partnership and teamwork
|
Attributes |
Generic standards |
FP Curriculum Syllabus Reference |
|
Communicate effectively |
|
6, 2, 3 |
|
6, 2, 3 |
|
|
6, 2, 3 |
|
|
2 |
|
|
Work collaboratively with colleagues to maintain or improve patient care |
|
7 |
|
3, 7 |
|
|
1, 7 |
|
|
19 |
|
|
|
|
|
|
Teaching, training, supporting and assessing |
|
4 |
|
1 |
|
|
|
|
4 |
|
|
|
4,6,7,8 |
|
|
|
19 |
|
Continuity and coordination of care |
a) Share all relevant information with colleagues involved in your patients’ care within and outside the team, including when you hand over care as you go off duty, and when you delegate care or refer patients to other health or social care providers. b) Check, where practical, that a named clinician or team has taken over responsibility when your role in providing a patient’s care has ended. This may be particularly important for patients with impaired capacity or who are vulnerable for other reasons. |
18, 20, 6, 7 |
|
|
qualifications, skills and experience to provide safe care for the patient. |
18 |
|
Establish and maintain partnerships with patients |
|
1 |
|
|
|
2 |
|
|
|
1, 2 |
|
|
a) Their condition, its likely progression and the options for treatment, including associated risks and uncertainties. b) The progress of their care, and your role and responsibilities in the team. c) Who is responsible for each aspect of patient care, and how information is shared within teams and among those who will be providing their care. d) Any other information patients need if they are asked to agree to be involved in teaching or research. |
2, 6, 9, 10, 11, 19 |
|
|
|
3, 16, 17 |
|
|
You must support patients in caring for themselves to empower them to improve and maintain their health. This may, for example, include: a) Advising patients on the effects of their life choices and lifestyle on their health and well-being. b) Supporting patients to make lifestyle changes where appropriate. |
|
|
|
|
1,6,18 |
Domain 4 – Maintaining trust
|
Attributes |
Generic standards |
FP Curriculum Syllabus Reference |
|
Show respect for patients
Treat patients and colleagues fairly and without discrimination |
|
1, 2 |
|
1,3 |
|
a) Put matters right (if that is possible). b) Offer an apology. c) Explain fully and promptly what has happened and the likely short-term and long-term effects. |
6 |
|
|
9 |
|
|
|
|
1, 9 |
|
|
|
2, 3 |
|
|
|
1 |
|
|
|
3, 10 |
|
|
|
6 |
|
|
|
2, 3 |
|
|
|
3 |
|
|
|
3 |
|
Act with honesty and integrity
|
|
|
|
Honesty |
|
2 |
|
18 |
|
|
1, 20 |
|
|
|
|
|
|
Communicating information |
|
6, 18 |
|
Openness and legal or disciplinary proceedings |
|
1, 6 |
|
1, 6, 18 |
|
a) You must take reasonable steps to check the information is correct. b) You must not deliberately leave out relevant information. |
1, 6, 18 |
|
|
|
|
|
|
Communicating information |
a) You must take reasonable steps to check the information. b) You must not deliberately leave out relevant information. |
1, 3 |
|
3 |
|
|
|
|
1, 3, 18 |
|
|
a) You have accepted a caution from the police or been criticised by an official inquiry b) You have been charged with or found guilty of a criminal offence c) Another professional body has made a finding against your registration as a result of fitness to practise procedures. |
1 |
|
|
|
1 |
|
Honesty in financial dealings |
|
1 |
|
|
|
1, 13, 14 |
|
|
|
2, 18 |
|
|
|
3 |
Appendix D: Curriculum development and list of contributors
This planned revision of the foundation programme curriculum (FPC) has been undertaken as an evolutionary process and has been performed with input and feedback from many stakeholders. During the revision there has been dialogue between representatives from the Academy of Medical Royal Colleges Foundation Programme Committee (AFPC), UK Foundation Programme Office (UKFPO) and General Medical Council (GMC) to ensure that changes are deliverable and that the regulator is aware of the nature of the revisions to ensure that they are in keeping with regulatory requirements.
This revision continues to reflect suggestions made in Foundation for Excellence: An Evaluation of the Foundation Programme report (2010) in particular in relation to the assessment process.
As a prelude to the revision process, feedback on the foundation programme curriculum was sought from a wide range of stakeholders both by direct invitation (key stakeholders and organisations/individuals who had previously expressed interest in the foundation programme curriculum) and by general invitation through the Academy of Medical Royal Colleges website. Extensive feedback was received, this was collated and emerging themes were identified. The curriculum working group reviewed the collated evidence and made revisions to the curriculum accordingly. There was a clear message of support for the changes made in 2012 and a request that changes introduced for 2016 should be evolutionary.
Based on the recommendations of the working groups, the AFPC assembled the draft foundation programme curriculum (the curriculum) which was sent for stakeholder review in 2015. After assimilation of these comments the revised draft was agreed by the AFPC and thereafter sent to the regulators for approval.
Undergraduate and postgraduate trainers, as well as organisers of training, were included in these consultations. The opinion of foundation doctors was sought from the Academy Trainee Doctors' Group, the British Medical Association Junior Doctors Executive Committee, the BMA Medical Students Committee and the UKFPO Foundation Doctors' Board.
The Academy of Medical Royal Colleges Foundation Programme Committee will continue to review and evaluate the curriculum. A further rewrite is scheduled to take place in 2021. Evaluation of the curriculum will be included in each local education and training boards (LETB)/deanery quality management process and the QAFP mechanism will monitor this.
Assessment in foundation
Dr Ed Neville (Chair), Dr Alan Connacher, AFPC/RCPE; Dr David Kessel, AoMRC Foundation Programme Committee/Royal College of Radiologists; Ms Susan Redward, General Medical Council; Dr Andrew Whitehouse, Associate Postgraduate Dean and Head of Foundation Programmes, HEWM Foundation School Director; Ms Stacey Forde, UKFPO, Dr Clare Van Hamel, UKFPO; Andrew Todd, Royal College of Physicians and Surgeons of Glasgow; Aileen Sced, Associate Dean HE Wessex; Jon Scott, Foundation School Director; Ms Johanne Penney, AoMRC; Bridget Langham, Foundation School Director ; Charlie Williams, Foundation Doctor; Eleanor Turner-Moss, Foundation Doctor and Nirja Joshi, Foundation Doctor.
Syllabus
Dr David Kessel (Chair), Dr Alan Connacher, AFPC/RCPE; Dr Helen Cugnoni, College of Emergency Medicine; Ms Johanne Penney, AoMRC; Dr John Lowe, Royal College of Psychiatrists/AoMRC Foundation Programme Committee; Ms Susan Redward, General Medical Council; Dr Emma Young, College of Emergency Medicine; Mike Masding, Head of Foundation School; Dr Rosemary Howell, Royal College of Obstetrics and Gynaecology; Dr Clare Van Hamel, UKFPO; Dr Helen Cugnoni, College of Emergency Medicine ; Dr Emma Young, College of Emergency Medicine; Stacey Forde, UKFPO; Simon Maxwell, Medical Schools Council; Jon Scott, Foundation School Director; Anthony Choules, Foundation School Director; Dr Charlie Williams, Foundation Doctor; Dr Eleanor Turner-Moss, Foundation Doctor; Nirja Joshi, Foundation Doctor; John Lowe, RCPsych and Matthew Walters, Scottish Deans Medical Education Group.